Putting Your Best Foot Forward
Footwork is essential to successful fencing. Take care of your feet! Junior men's saber final, Summer Nationals 2024. Photo: Serge Timacheff
The human foot is one of the most versatile parts of the body. It plays a significant role in stance, balance and ambulation. The human foot can be compared with the treads on a bulldozer. There is a certain about of rigidity for leverage combined with flexibility allowing for wide-ranging adaptations to various surfaces and terrains. The foot comprises 26 bones connected by a complex network of connective tissues, ligaments and muscles. With constant changes in stance, balance and a variety of movements, fencing is a sport that predisposes its participants to repetitive movements.
Foot injuries are some of the most common sustained to athletes affecting one’s ability to perform at their highest level. The purpose of this article is to explore common injuries and conditions and provide some helpful guidelines in helping you care for these ailments at home. As with most injuries and conditions, if self-care does not result in a quick resolution, scheduling an appointment with a qualified sports medicine practitioner is recommended.
Calluses
Calluses can affect fencers of all ages and skill levels.
Calluses are common problems that bother fencers of all ages. They are caused by excessive friction, often from improperly fitted shoes. If the buildup of a callus is not controlled, it can become susceptible to tears, cracks, blisters and possible infections.
Management of Calluses
If one has recurrent calluses, prevention is the key. Use of a callus file to keep the callus small is encouraged, yet do not completely remove the callus as some of it is needed for protection. The best time to file a callus is after showering.
Apply a small of amount of moisturizer such as Aquafor, Bag Balm or petroleum jelly to maintain or facilitate tissue elasticity.
Wear at least one layer of clean, cushioned socks. Ensure there are no creases, folds, or wrinkles.
Wear properly fitted shoes that are in good condition.
Preventively apply petroleum jelly or other lubricant to minimize friction.
Blisters
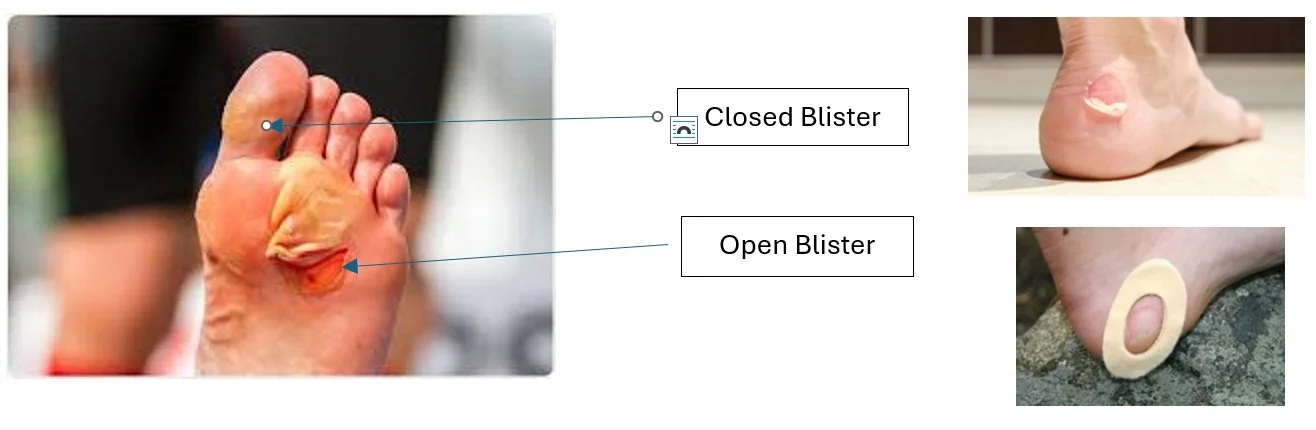
Blisters can be some of the most annoying and debilitating injuries in sports. Blisters are minor skin injuries caused by repeated shearing forces and friction presenting with the feeling of a hot spot, burning and/or pain resulting in a raised area filled with clear fluid or blood. The best approach in treating blisters is prevention. Prevention and initial care are paramount to addressing the environment that causes blisters. Using petroleum jelly can be helpful in prevention, and wearing properly fitted shoes and socks is essential. Additionally, new shoes should be broken-in before being worn for long-term practices or competitions.
Blisters: One of the most annoying and debilitating injuries in sports.
If a blister or hot spot develops, the athlete should cover the area with lubricant, moleskin or a friction reduction bandage. Using powders, lubricants and padding counteract the effects of the stress on the skin. Additionally, wear appropriately fitted shoes and two pairs of socks.
If a blister develops, try to leave it intact, and if possible, keep the area dry and clean. Appropriately pad the area to disperse the pressure and protect the area.
Management of Blisters
Closed blisters require maximum protection with lubricants, Second Skin and padding
Open blister
Must be treated as an open wound
Clean the area with saline or soap and water
Appy triple antibiotic ointment under and around the loose skin
Cover with sterile bandage and apply donut pad to disperse the pressure
Change dressing daily
Contusions are bruises caused by high stresses on the heel.
Heel Contusion
Fencing is a sport requiring stop-and-go responses along with side-to-side and up-and-down movements. These dynamic actions place high stresses on the heel, which has a thick, natural fat pad providing natural cushioning. However, the nature of fencing actions predisposes this padding to unnatural stresses that may result in a disabling contusion or bruise to the heel.
Management of Heel Contusion
Initial care with ice
Limit excessive weight bearing activities for 24-48 hours
Incorporate use of padded heel cup, donut pad or taping for initial care and prevention
Padded heel cups and donut pads help alleviate pain and encourage healing for contusions.
Ingrown Toenails
An ingrown toenail is a condition in which the edge of the toenail grows into surrounding soft tissue. The classic symptoms of an ingrown toenail include heat, swelling, redness, pain and an accumulation of pus. As with other conditions affecting the foot, prevention is key. Properly fitted shoes will prevent constant pressure on the toenail that leads to irritation. Properly trimmed nails will also prevent problems. Nails grow to the areas that are thinnest. Cutting the nail straight across and not curved will help. The nail should also clear the underlying tissue.
Management of Ingrown Toenails
Ingrown toenails can cause intense, localized pain and discomfort.
Soak the toe in warm water for 15-20 minutes 2-3 times per day. Adding Hibiclens, Betadine, or other antiseptic solution to the water will help combat any infection.
With the skin and nail softened, place cotton or gauze under the edge of the nail to lift it away from the skin. Continue this until the nail grows out and is able to be trimmed straight across.
If the toe becomes infected or is not improving, get medical attention.
Plantar Fasciitis
Plantar fasciitis is one of the most common foot problems seen in athletes. It may result from extrinsic factors such errors in training, sudden increases in workload, change in exercise environments, improperly fitted or worn footwear and participation on unyielding surfaces such as fencing strips. Additionally, there are intrinsic factors that may lead this condition manifesting itself, including high arches (pes cavus), flat feet (pes planus), decreased strength of the muscles of the lower leg and foot and decreased flexibility of the calf muscles.
When an athlete presents with plantar fasciitis, one of the most common complaints is severe pain with the first few steps in the morning. The pain will be most isolated to the inside (medial) bottom of the foot closest to the heel. The pain will usually decrease with activity but will return after a period of rest.
The best way to address this condition is to engage in flexibility of the calf muscles and muscles of the foot, massage and other soft tissue manipulation, and strengthening of the muscles of the foot.
Management of Plantar Fasciitis
In initial stages, use of ice and non-steroidal anti-inflammatory medication
Use a shock-absorbing heel pad such as a Tuli
Roll foot on lacrosse ball or closet dowel
Implement Achilles tendon stretching
Leg straight
Leg bent
Stretches should be comfortable and held for 30 seconds. Do three repetitions three times daily
Use of a night splint
Strengthen the muscles of the foot
Towel crunches
Marble pickups
Maintenance of general body fitness
Achilles Tendonitis
Disorders affecting the Achilles tendon are common maladies affecting fencers. As with plantar fasciitis, Achilles tendon disorders result from both extrinsic and intrinsic factors. The combination of these factors causes micro-traumatic changes from the forces exerted by the calf muscles that result in inflammatory damage to the structural fibers of the tendon.
Someone suffering from an acute (fresh) injury to the Achilles tendon will experience aching or burning on the back of the heel where the tendon attaches into the heel bone (calcaneus) as well as discomfort with stretching and going up on the toes. There will be associated tenderness when touching the tendon as well as areas of localized swelling. If the tendon is not treated in the early stages of the irritation, it can progress to a long-term/chronic problem. The tendon will thicken and the pain will become more diffused. Additional changes may result in bony malformations such as excessive calcification and bone spurs.
As with all injuries, the goal of treatment is to minimize pain, improve flexibility and strength and return to full, unlimited pre-injury levels. Stresses applied to the injured area should be gradual and care should be taken to prevent further degeneration and degradation of the tissue.
Management of Achilles Tendinitis
Primary objective is to minimize pain, prevent further damage, and gradually return to unrestricted participation
Active rest to include full body conditioning
Use of ice and non-steroidal anti-inflammatory medication
Implement Achilles tendon stretching
Leg straight
Leg bent
Stretches should be comfortable and held for 30 seconds. Do three repetitions three times daily
Gastrocnemius and soleus (muscle to form the Achilles tendon) strengthening
Summary
The foot functions to absorb shock and provide a stable base of support during walking, running and jumping — and all-important footwork in fencing. The foot comprises 26 bones held together by a network of ligaments and muscles. Most injuries and conditions affecting the foot can be prevented through proper footwear and proper hygiene. Preventive self-care can go a long way to allow you to participate at a high level. However, if a problem persists or progresses, it is advisable to schedule an appointment with a qualified sports medicine provider.